Sunday, July 20, 2008
mrcp,rheumatology
30 years old male got acute left knee arthritis with swelling.it gradually resolving for 2 months and now he got acute swelling and tenderness in right knee.no history of eye redness or dysuria.no history of gonococcal urethritis.no back pain.
mrcp,rheumatology
A 30 year-old man is admitted to casualty with a 24 hour history of a painful and swollen right knee. He denies any previous history of joint problems. Over the last two days, he has also noticed redness and soreness in both eyes. He has returned from a business trip to Kuala Lumpur a fortnight ago.
On examination, his temperature is 38.5°C. His eyes are red. His right knee is hot, swollen and tender to palpate. No other joint appears to be affected.
Investigations:
Hb 12.9 g/dl
WBC 14.0 x 109/l
Platelets 200 x 109/l
ESR 75 mm/h
Blood cultures
No growth after 48 hours
Urinalysis
No blood, glucose or protein detected
Knee x-ray
Soft tissue swelling around left knee
What is the most likely diagnosis?
1 )Gout
2 )Gonococcal arthritis
3 )Reiter's syndrome
4 )Rheumatoid arthritis
5 )Viral arthritis
On examination, his temperature is 38.5°C. His eyes are red. His right knee is hot, swollen and tender to palpate. No other joint appears to be affected.
Investigations:
Hb 12.9 g/dl
WBC 14.0 x 109/l
Platelets 200 x 109/l
ESR 75 mm/h
Blood cultures
No growth after 48 hours
Urinalysis
No blood, glucose or protein detected
Knee x-ray
Soft tissue swelling around left knee
What is the most likely diagnosis?
1 )Gout
2 )Gonococcal arthritis
3 )Reiter's syndrome
4 )Rheumatoid arthritis
5 )Viral arthritis
erythema nodosum,mrcp


Very frequent MRCP exam question, especially Part 1 & 2a, don't be surprised if it comes out in Station 5 PACES.
The picture shows erythematous nodules over the legs involving the shin. They are tender and elevated.
My diagnosis is that this patient has erythema nodosum.
You need to know the causes !
May even appear in history taking if you read Mir &Ryder PACES
Idiopathic/ unknown
Sarcoidosis
Streptococcal infection
Tuberculosis
Infections other than TB or strep - HIV...
Pregnancy or oral contraceptives
Drugs other than OCAs
Inflammatory bowel disease
Behcet's disease
Other
massive splenomegaly.+mrcp
Box 1 Diseases that cause massive splenomegaly.
- Chronic myeloid leukemia
- Extrahepatic portal vein obstruction
- Gaucher's disease
- Hairy-cell leukemia
- Idiopathic portal hypertension
- Malaria
- Malignant lymphoma
- Myelofibrosis
- Thalassemia major
- Visceral leishmaniasis (i.e. kala azar)
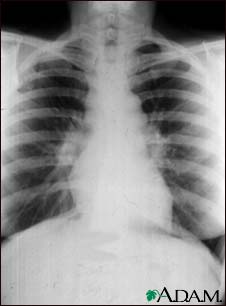
sarcoidosis in mrcp
They would usually show show you a CXR in MRCP
Remember that 90% of CXRs have bilateral hilar LN enlargement. More advanced case may have diffuse fibrosis!
Tips for MRCP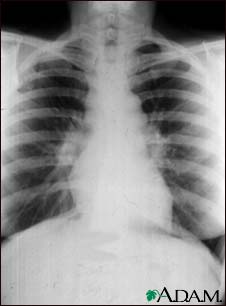
Remember that 90% of CXRs have bilateral hilar LN enlargement. More advanced case may have diffuse fibrosis!
Tips for MRCP
1) If you are asked about a patient with painful skin lesions over shin area with dry cough, always think of sarcoidosis.
2) A patient with high calcium level and dry cough , think of sarcoidosis although there is possibility of lung cancer with bone metastasis!
- Stage 0 is a normal chest x-ray.
- Stage 1 is a chest x-ray with enlarged lymph nodes but otherwise clear lungs.
- Stage 2 is a chest x-ray with enlarged lymph nodes plus
infiltrates (shadows) in the lungs. - Stage 3 is a chest x-ray that shows the infiltrates (shadows) are present but the lymph nodes are no longer seen.
- Stage 4 shows scar tissue in the lung tissue.
Subscribe to:
Comments (Atom)



