Disease as expressed in the face and posture.
Facies cardiac (heart): An anxious expression seen in the early stages of chronic valvular disease.
A purple or bluish appearance of the face, especially about the eyes, temples, and ears, with veins showing on the nose and sometimes on the cheeks, intensified by lying down: Caused by high blood pressure and an approaching dangerously plethoric state of the body.
Hepatic face: An earthy appearance; yellow tinge, jaundice.
Hippocratic face: Indicating rapid approach of death--pinched nose; hollow temples; eyes sunken; ears leaden and cold; lips relaxed; skin livid, and if the skin is pinched it returns slowly to the plane from which it was pinched or drawn.
Ovarian face: Features emaciated and sunken; anxious expression; forehead furrowed; eyes hollowed; nostrils open and sharply drawn; lips full and compressed; angles of mouth drawn and wrinkled, puckered but protruding"fish mouth."
The stupid face is that of typhoid.
Gastric face in children: A white line around the mouth, extending up by the side of the nose, shows irritation from improper feeding. Add to this sign pungent breath and vomiting, and the child has gastritis.
Gastric face in adults: Chronic irritation of the stomach in adults is indicated by a dragging-down of the comers of the mouth. Add to this drooling or driveling of saliva, and the indication is of starch poisoning; and if there is a broad, pallid tongue, the evidence is strong for overeating on starch.
Hysteria is marked by staring and an ecstatic expression.
Epilepsy is marked by a stupid face after an attack.
Protruding eyes and expressionless face in Graves' disease.
They lypermaniac has sadness written in his face. In general paralysis the countenance is composed and satisfied. The enebriate has trembling bps and a wandering expression.
The child with enlarged tonsils and adenoid growths has a stupid expression; the mouth is open, the lips hanging; the nose is expressionless.
The red nose, enlarged veins, bluish lips, cyanosed cheeks, and puffiness of face of the drinking man are called the mitral face. Where the aorta is diseased there is intense pallor. In Bright's disease the face is swollen and white.
The signs of croup are well known, but the type of disease is not so easily told. There are coughing and suffocating when a foreign body is in the air-passage.
Expiratory disturbance is marked by flushed face, puffed and bluish; the eyes are suffused, and the veins stand out.
In marasmus the features are drawn, the furrows deepened, the neck hollow; emaciation is marked, and, when profound, the whole appearance is that of the monkey.
The consumptive appearance is that of emaciation; protruding, flushed cheeks; pinched nose, with flaring nostrils; short, quick, jerky breathing; halting speech, and more or less suppressed voice.
When the face looks smaller--shrunken--and the nose is thin, long, and drawn, the bones prominent, the skin pale and covered with cold sweat, and, when drawn or pinched, the fold remains for some time, this is the facies of peritonitis, intestinal obstruction, renal and hepatic colic.
Fainting: The heart stops; the patient turns pale and falls motionless, but there is no distortion of the face; breathing is suspended.
Apoplexy: The patient is motionless and lies on the back; all animation is suspended; only breathing and pulse continue; the breathing is noisy, and gradually grows more stertorous. If the patient does not react and improve, the breathing and heart action gradually decline, the skin becomes drawn, the nose thinner and longer, the eyes dull, partially closed, glassy. The breathing stops, starts and continues, until it finally ends with a slight bodily convulsive movement.
Physical appearance must be noted--all deviations from the normal mean something.
Deformities, such as rickets, shorten the stature and cause the head to appear too large; the spine is incurved, the pelvis is deformed, the limbs are curved, the ribs project forward.
When the muscles become atrophied they cause general deformity.
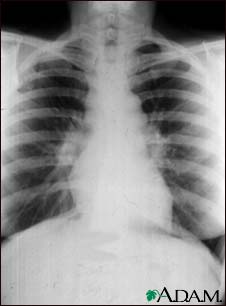
Alterations of the heart or lungs cause deformities of the chest.
The bowels are often too large and distended from gas, fat, or ascites; in fevers, from tympanitis and inflammations.
Enlargement of the liver or spleen causes a large abdomen in the upper region; in the lower abdomen, enlargement may come from tumors, distended bladder, or a gravid uterus.
A large swelling at the base of the great toe, with the toe pointing outward, indicates a bunion. This deformity usually means that there is a slight rheumatism. Deformity of the third joint of the fingers--nodes of Heberden--means arthritis deformans. The nodes of Bouchard on the second joints of the fingers indicate dilation of the stomach--a disturbed nutrition from overeating of the carbohydrate foods. Joint distortions indicate gout, rheumatism, or injury; not infrequently they mean all of these. Frequently injury is complicated by rheumatism.
Hippocratic fingers (clubbing of finger-tips, with incurving nails) indicate heart or lung disease--scrofulous diathesis.







 RA hands: symmetrical deforming arthropathy with synovial thickening.
RA hands: symmetrical deforming arthropathy with synovial thickening. Psoriatic arthropathy: asymmetrical arthropathy involving terminal IPJ with nail changes.
Psoriatic arthropathy: asymmetrical arthropathy involving terminal IPJ with nail changes. Chronic tophaceous gout: asymmetrical deforming arthropathy with tophi formation.
Chronic tophaceous gout: asymmetrical deforming arthropathy with tophi formation.






















acromegaly disease is active or not, what is the full answer?
sweating, hypertension, glycosuria and headaches will indicate disease activity